Interview with Dr. Joe Sherman
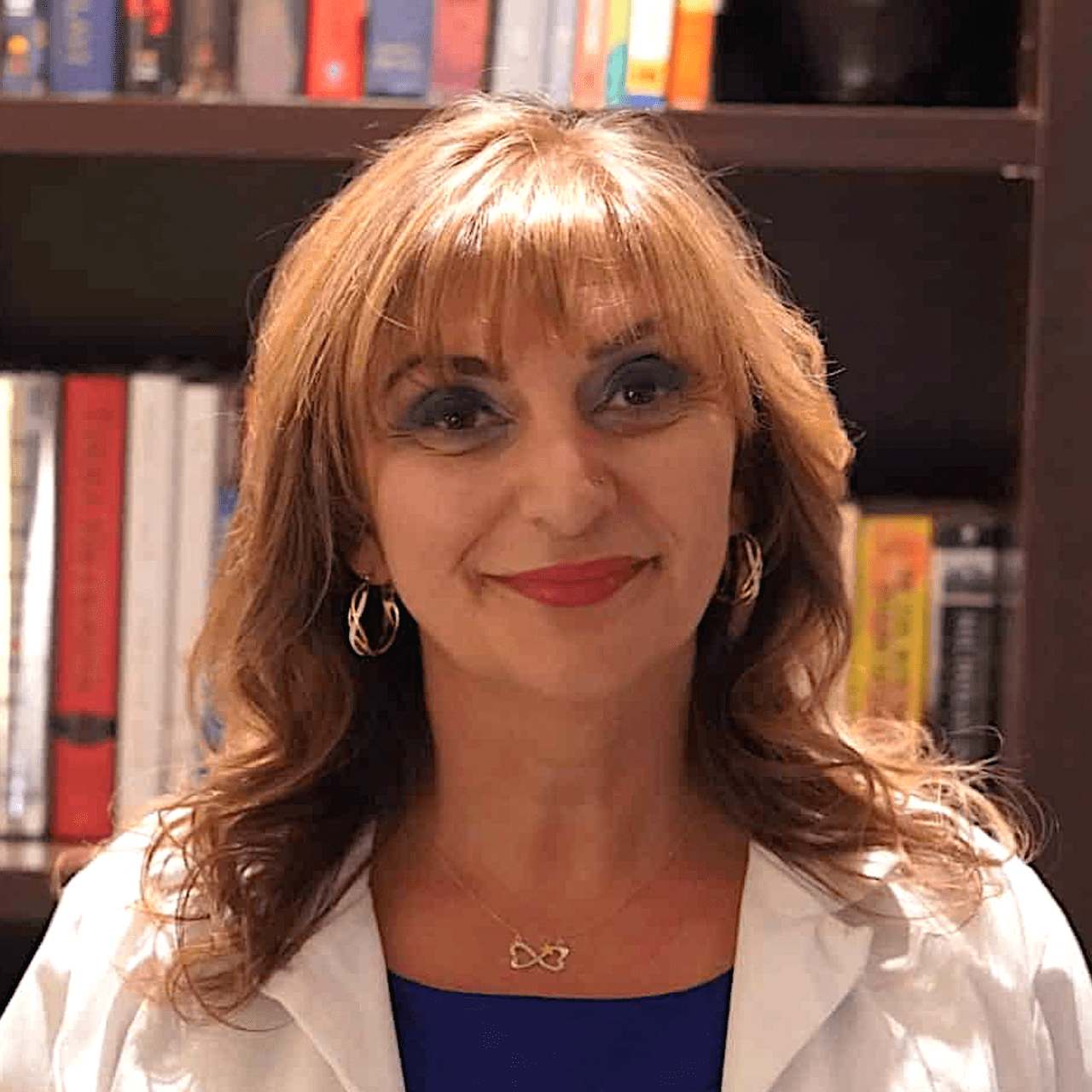
In today's podcast, Dr. Joe Sherman describes how he helps physicians align ‘soul to role' during their career selection process.
By avoiding burnout and broadening possibilities, Dr. Joe Sherman, a physician coach and retreat leader, helps other doctors discover greater joy in their lives.
Joe obtained his medical degree and residency training in pediatrics at the Virginia Commonwealth University School of Medicine. And for more than 30 years, he has provided healthcare to children in the District of Columbia, Tacoma, Seattle, Uganda, Bolivia, and other nations.
He recently served as the Health Services Director at Mary's Place, a refuge for homeless families. At the University of Washington in Seattle, where he currently holds a clinical associate professorship in pediatrics, he has held a number of academic positions.
Our Sponsor
We're proud to have the University of Tennessee Physician Executive MBA Program, offered by the Haslam College of Business, as the sponsor of this podcast.
The UT PEMBA is the longest-running, and most highly respected physician-only MBA in the country. It has over 700 graduates. And, the program only takes one year to complete.
By joining the UT Physician Executive MBA, you will develop the business and management skills you need to find a career that you love. To find out more, contact Dr. Kate Atchley’s office at (865) 974-6526 or go to nonclinicalphysicians.com/physicianmba.
Align ‘Soul to Role' During Career Selection
The idea in Parker Palmer's book “Let Your Life Speak,” to align your soul and your work (or role), resonated with Joe. Examining past experiences and reflecting on them can help us discover the things that truly make us happy.
Joe was drawn to the Center for Courage & Renewal after reading the book by Palmer, one of the Center's founders. He began coaching physicians and holding retreats for those seeking guidance on how to live more realistically.
Dr. Sherman's Retreat
The Center for Courage & Renewal's traditional concept involves gathering people together for four days to form a community. Participants work on their individual problems in a circle of trust with a set of rules known as touchstones. Much of the work is devoted to career selection.
Joe offers half-day or full-day mini-retreats for inpatient medical teams, or outpatient clinic workers. He creates also provides reflection groups or workshops, along with the traditional retreat, in locations where one can reflect, rest, and revitalize while earning CME credit.
Summary
You can access a free 30-minute consultation on his website: joeshermanmd.com. During that consultation, you will look at your life, and reflect on how it worked or didn't work. Additionally, you can email him at joe@joeshermanmd.com.
Dr. Sherman's next retreat will be held on Whidbey Island, Washington, from September 22 through 25, 2022. In addition to working on aligning your “sole to role,” during career selection, members participate in kayaking and other mountain activities in a stunning setting with the breathtaking Olympic Mountains in the distance.
NOTE: Look below for a transcript of today's episode.
EXCLUSIVE: Get a daily dose of inspiration, information, news, training opportunities, and amusing stories by CLICKING HERE.
Links for Today's Episode:
- Dr. Joe Sherman's Website
- Joe Sherman, MD, Workshops
- Let Your Life Speak by Parker J. Palmer (affiliate link)
- Center for Courage and Renewal
- Find the Fulfillment of a Freelance Remote Yoga and Meditation Teacher – 250
- Can Meditation Offer Help for Burned-Out Physicians? – 172
- NewScr!pt
Download This Episode:
Right Click Here and “Save As” to download this podcast episode to your computer.
Podcast Editing & Production Services are provided by Oscar Hamilton
Transcription PNC Podcast Episode 260
Boost Well-Being by Aligning 'Soul to Role' in Career Selection
John: Today's guest is an accomplished pediatrician. In fact, he's done his pediatric practice all over the world from what I can tell, but really that's not why he's here today, because he's transitioned into being a coach, consultant and retreat facilitator, which we're going to learn about today. So, with that, I would just like to welcome Dr. Joe Sherman. Hello.
Dr. Joe Sherman: Hi John. Thanks so much for having me.
John: It's my pleasure. I'm looking forward to talking and hearing about your burnout, how you transcended that or overcame that and what you're doing now. So, it's going to be a very interesting conversation, I'm sure.
Dr. Joe Sherman: Yeah. Thanks so much. I always enjoy talking about this.
John: Excellent. So now we usually start with a little background. Just give us the short version of your background, your education, clinical work, and definitely touch on some of the things you've done that are a little different from the typical pediatrician.
Dr. Joe Sherman: Sure. I'm an east coaster. I was born and raised in Washington, DC in the city and went away for college at Duke University and then went to Richmond, Virginia at Virginia Commonwealth University, Medical college of Virginia. I did both medical school and residency there in pediatrics and then moved from there back to DC and then began my career as a general pediatrician.
And I would say that the majority of my focus in practice was service to underserved populations of children and families. And my passion really lies in the education and teaching of trainees and bringing the community and the academic center together in trying to link them up. And back then in the late 80s, when I was beginning my practice, most training centers were ivory towers and you never left the building. Now it's a little bit more integrated, but at the time it wasn't.
I worked in many outreach projects where we had teams, interdisciplinary teams to reach out to different populations, pediatric mobile clinics and teams that were based in the community and doing house calls and so forth. In addition to that, I've had stints in Uganda as well as in Bolivia. And I love international health and working with organizations in both of those countries, as well as short term trips to some other Latin American countries.
So, that's about a summary of my clinical experience. And as long as I kept doing that variety of things, I found that I was fulfilled in medicine. But I have to say that pretty much the whole time, even at the beginning of my training, in the back of my mind there was always this thought that came up of "Does this have to be in medicine? Could I be doing some of these things outside of medicine?" Because I always enjoyed athletic coaching and counseling and tutoring and mentoring. And so, those are the things that, especially overseas where you have to kind of wear a lot of hats when resources are very low. That's when I found that I really thrived.
John: Nice. You were sort of going back and forth in some of these activities but apparently from our conversation before we got on the call here, is that you at some point had some episodes where you were pretty burnt out, is that right?
Dr. Joe Sherman: Yes. I would say I was. And I think the classic definition of burnout, this emotional exhaustion dissociation, sense of lack of impact and so forth. At times I had that classical syndrome, I would say. At other times I feel like I was just misplaced, perhaps. It was just the wrong job with the wrong time in my life. And during my time in my practice, I went from being single, to being married without kids to later on being married with kids and little kids and then big kids. Life changes, your situation changes. So therefore, what you're attracted to as far as a practice, a job, an activity is concerned, also changes. I had some minor changes and I always kind of switched jobs I think in those situations and moved on. Opportunities were there.
But then the real crash came when I returned from Bolivia after living there for four years with my family and we raised our little kids there. And returned and tried to plug back into academic medicine here in Seattle. And I just started to go downhill and it was confusing to me. I know that what I had experienced in Bolivia was amazing. I was doing a variety of activities and that fit me well. And yet when I was placed in this clinic in an atmosphere and setting that it seemed like logically, cognitively on paper, would've been the perfect fit. I found myself going downhill. It was confusing to me. I became increasingly anxious. I wanted to work harder to try to fix a broken system. I felt responsible for everybody and everything.
And so, at a time where I was really starting to feel uncertain, it was proposed to me that I was doing such a great job. Why don't I become the medical director of the clinic? And so, like many of us physicians do, when we think something's wrong and we're not feeling too well about our situation, we work harder to try to make it better and try to fix it. And so, I did, and that just made me crash even further.
John: After speaking with so many people about this topic, I think there's an expiration date or something sometimes. Sure, there's medical students, residents they're burned out from day one. They stay burned out and they get fried, but most of us go into it, we're excited. It's interesting. We're at the top of our game because we've just finished our training. I don't know. It's almost like a candle. There's a point where the candle is gone. It's disappeared. The wax evaporated, it burned and there's nothing left And for each of us, medicine is such a fast-changing field that it's really easy to get overwhelmed. And you can only keep that level of intensity for so long. So, I don't know. That's kind of what I'm starting to think about after going back and thinking about my burnout.
Dr. Joe Sherman: Yeah. John, I think as I look back during the time of my training and then my medical practice, medicine has changed dramatically during that time. I mean, not just the evolution of the electronic health record, but also other technology and research and the complexity of medicine has changed. And so, the things that I could keep in my little pocket of that handbook that said, "Oh, I'll just look it up in the Harriet Lane Handbook and tell you what to do." Now it's an enormous amount of information.
John: It is. And I think about this all the time. When I was in med school, literally there were probably 10 medications I had to choose from. A couple of antibiotics, Lasix. Tegnect, the first medicine for ulcers. It didn't exist when I started med school. It's just overwhelming now. There's like a bunch of drugs for COVID. It's just blowing my mind. I can't keep up. Anyway, I'll stop beating that horse.
Dr. Joe Sherman: I'll just say there was just one little vignette very quickly, is that when people talk about HIV. HIV now.
John: Oh yes, exactly.
Dr. Joe Sherman: I had one hour lecture on HIV in my entire medical career, in my entire medical training. And it was by a pathologist who just said there's this strange disease seen in San Francisco. Just want to let you guys know and stay tuned for more. That was it.
John: Wow. Well, I think about that and I look back and I had two patients die of HIV, no treatment whatsoever available for it. And now it's like, okay, we've got these multiple drug pills you take once a day, once a week, whatever. And it's completely controlled. So, it's fantastic. But boy was that frustrating back in the day.
Dr. Joe Sherman: My first pediatric patient, it was a baby who died of perinatal transmission of HIV.
John: That's rough. Okay. Now, you kind of did a reassessment and started to think about whatever the next thing you were going to do when you decided, "Well, maybe I've reached that point." So, tell us about that transition and what you did to prepare for it.
Dr. Joe Sherman: Sure. Like I say, I tried to hang on and make things better. And I was in therapy, seen a psychiatrist just because of anxiety, depression, but still would not let go of this job because it was my identity. And finally, I had to. It was kind of like if I wanted to stay in my marriage, in my family, I just had to do something. So, I did. And it was a time where I stopped and just sat back and said "I need to really reassess where I am in my life and how I got here."
And I came across a book written by Parker Palmer called "Let Your Life Speak." And he wrote about this concept of soul to role that somehow we can examine our lives and see the experiences that we've had and from looking at those experiences we can reflect on that and determine what are those things that really bring us joy in life. What are those things that really bring us to life that make us feel like we are excited?
One of the things that I say is what is some activity that while you're doing it, you wish it would never end because you're having so much fun or you're enjoying it so much? Or what is something that you have done that you say, "I can't wait to get back and do that again?" And then extract the elements of what was present in that time and see how that might fit into a career or your next decision or other things in your life.
Reading that book attracted me to the Center for Courage & Renewal, which is a center that he helped found and group retreats for people who were trying to discern how to live their lives more authentically. And so, I went to a couple of those retreats and found them extremely helpful and decided to train to be a facilitator of those retreats. And that's how I got my start with accompanying health professionals on that journey.
John: Okay. Yeah. Tell us about the retreat concept, maybe the way you're doing it now, or how it's evolved for you. I've always found that group activities can be very helpful because people have the shared experience, but yet they have their own perspective and they've learned and they can learn from one another. So, what's that been like for you? How would you do that? Do you get a group of doctors together?
Dr. Joe Sherman: Yeah. The classic model for the Center for Courage & Renewal is this. Go away to a place for like four days and come together and establish community. It's almost parallel reflection, parallel discernment. And so, everyone is working on their own issues, but you're doing it in a circle of trust, a circle that has a certain guideline you call them touchstones.
Well, the problem is healthcare professionals are very busy. It's really hard for them to get away for that much period of time. So, I tried to adapt it a bit to their situations. I started to do mini retreats for medical teams, inpatient teams, such as palliative care teams or outpatient clinic staff and say, "Hey, let's do a half day retreat or all-day retreat." Or the other thing that I did was, for example, with palliative care teams, can I meet with the team for an hour and a half once a month and have this ongoing reflection on their experiences and how it applies to the direction that they want to take. And this builds team unity and also helps people understand each other on the teams.
Those are types of offerings that I have now, which are those short term, either reflection groups or workshops, as well as the classic getaway and do in that model of going to a place where you can reflect, you can relax, you can rejuvenate, and you can also gain some CME credit for it at the same time. So, we also have those available too.
John: Okay. I think you've got one coming up in a month from what I remember, a month or two. Who would be the ideal member or someone who would come to that? In other words, are you bringing a team from one local spot or are you pulling people from the whole country? And what is the thing that is common to all those people where getting together is going to help them?
Dr. Joe Sherman: Yeah. I have a co-facilitator who's a clinical psychologist who specializes, all of her clients are physicians. These retreats that we have, that we co-facilitate together, we have one in the wintertime in February that's in Florida. And then we have one that's in the early fall on Whidbey Island outside of Seattle, Washington. And these retreats are transformational leadership retreats. And they're worth 25 hours of CME credit, category one credit. And it's really a time for any type of physician, nurse practitioner, PA, medical provider, who wants to examine their practice, their lives in the context of a position that they hold. Perhaps it's a leadership position, either formal or informal within their organizations. And the idea is "I want to examine what brings me life and how I can act more authentically and then how I can transform my organization so that I can provide a space and a culture for everyone to be able to do that."
And one of these big AMA surveys that was done during the pandemic concluded that there were two elements that were associated with resilience of medical providers during the pandemic. And those two elements that had to be present in their organization was one that they felt like there was a shared mission that they felt like they were all in this together. And that that was explicit and lived out.
The second was that they felt valued, that they felt like they were valued by their organization as a member of that organization. And that has implications. The implications are that you're engaged in decision making and the direction that things take. So, those are the topics that we deal with during these retreats as to how to get yourself to examine who you are, why you do what you do, and then how you can bring that to your organization.
John: I find that interesting and I have a question for you about that only because most people that I talk to on my podcast here are people that are ending up leaving medicine. But there's been coaches that I was surprised to find out during the interview that like 80%, 90% of the people they work with actually stay in practice. So, it's how they do the coaching or the people that are coming to them, but that's the whole point is they want to continue in practice.
What I'm hearing from you is that if you can become a leader in one of these organizations, you can continue doing what you're doing now. You may be pulled away and spend more time in leadership and less time seeing one on one patients. But is your feeling that most of these people are there to learn how to stay in practice with a group and support one another and continue doing that for patients?
Dr. Joe Sherman: I would say for these retreats, people come with all kinds of ideas because they're at different stages of their careers. Some people are early on, pretty young. Some people are looking at perhaps retiring and maybe they're burned out. Maybe they need some reason to stay in it, or maybe they're looking at a way to make it work. And making it work may be that they transition a little bit out of clinical medicine and more toward administration or more toward program development or something outside of clinical medicine altogether. It's different for every person I would say.
John: Do you get feedback from the participants later? What's your general sense of their ability to make that change?
Dr. Joe Sherman: Yeah. It's so hard because when I talk to physicians and other clinicians, they feel like they're stuck in a system that is intransient. It just will not change.
John: It's a system.
Dr. Joe Sherman: It's a system problem, right?
John: Yeah.
Dr. Joe Sherman: And usually my response to that is you're right. It is unjust to blame you as an individual physician or other provider. It's unjust to say, "It's all your fault. You just have to shape up, do a little meditation and yoga. You'll be better." That is totally unfair. We are in a broken system. Now, as a result of that, what are you going to do about it? If you are someone who is a political activist and you are a leader, and you're going to really put your energy into changing the system, all the power to you, we need more people like that. If you're not, and you really want to concentrate on taking care of patients or concentrate on teaching or research or whatever it is. Well, then what can you do to fortify yourself to make your own experience more fulfilling? And what can you do with the closest sphere of influence around you? Who do you interact with every day? Because those are the people that can make or break your day.
So, we focus on that. And I would say that when people go through our retreats, as well as my individual coaching, that's what I really focus on is really what is it that drives you and how can you bring that out in other people so that you provide a culture that everyone feels supported? They feel like they're valued, and they feel like they're in the same mission.
John: And when I left medicine, I went into administration at a hospital, became a chief medical officer. And so, I was kind of on a dark side in a way. But I think that while I was doing it, I was actually helping the physicians. Even at the base level of saying, "You know what? You're not getting paid enough. We're going to give you a raise" The CFO was not going to volunteer to do that. The CEO wasn't either. And so, I'm always encouraging people to get involved in leadership. If you're frustrated, you can go one of two ways. You can bail on the whole thing, or you can get involved and change it somewhat.
Dr. Joe Sherman: Yeah. I think what they used to say is that the MDs that go to administration went to the dark side and now we don't like them anymore because they're the bad guys. But it's almost like administrators and clinicians live in these two different cultures. And never the twain shall meet or get along, but I've been in situations, especially with smaller organizations where that shared mission is explicit and discussed amongst administrators as well as clinicians. And when you do that, then you want to learn from the other person.
And tell me about your experience. Tell me about the pressures as an administrator that you have to keep the bottom line going. And I'll listen to you as long as you listen to me about the hassles I have to do with trying to check all the boxes you want me to check. And I think if people are able to see each other as humans and move forward in that, then I think they can get along. And I also believe that money is not always the answer and it's turning out I think especially during this pandemic, that time and the quality of how you spend your time is so much more valuable to people.
John: Right. Absolutely. Anecdotally, I think there's evidence that large systems that are actually run by physicians, that understand one another, have more engagement with the other physicians and actually their burnout levels are lower. So, that's why I encourage physicians to get into those leadership positions because yeah, you can improve it even within a broken system.
Dr. Joe Sherman: Yeah. And I think sometimes it's intimidating and it's interesting because when I do individual coaching, individual coaching in the corporate business world is thought to be a perk. It's thought to be, "Wow, I got a coach. This is great."
John: That's right.
Dr. Joe Sherman: But for physicians, it's thought to be a little bit kind of like remedial, like you're behind in your charts, you're causing a problem in the OR, we need to coach you up so that you act better. So, when coaches, even when they get to leadership positions, sometimes they think "Coach? Oh, gosh. I don't want you to, because I just need to learn how to be an administrator. I need to learn business." And it may be true. You need to learn the vocabulary, but you're not in the room. There's plenty of business people in that room. They need people who can tell them this is the implication and the impact of that decision on the clinicians when you make that change.
John: Yeah. So many of them just really have no idea if they've never been a clinician at any level. There's a lot of nurses that run hospitals and that kind of thing. But when you have just the MBA, it's doing it. They really don't understand the physician-patient relationship or what a nurse really truly does. Okay. So now I want to pick your brain a little bit more because you mentioned the book earlier and you mentioned Let Your Life Speak and you mentioned Soul to Role.
Dr. Joe Sherman: Yeah, that's correct.
John: Which you explained, but can you give us a little bit more about how I might be able to figure that out? I'm one of those people like, I don't know how I feel and how am I going to figure out what I really enjoy doing?
Dr. Joe Sherman: Yeah. As physicians, we're very much in our heads all the time. And the strangest thing is that we deal with the body. I mean, that's what we're dealing with. We dissected it. We do study physiology, all that stuff. We're not very in touch with our own bodies. And we're not very much in touch with our emotions, our soul, whatever you want to call it.
A lot of times, I think "What are you talking about this solar role? What is it?" Well, one thing is to say, and what we talked about before is think of an experience that you've had where you've felt those things that I said, "I wish it would never end or I can't wait to do it again." And then you look at it and you say, "Wow, who was involved? What was the setting? What was it? What are the values I was living out? What were the feelings? How did it feel in my body? What were the emotions I felt?"
Now I have to say, for me, you have to be pretty elementary with physicians. They say with myself too. So, I have a list of emotions, a list of feelings, a list of body sensations. Pick something, circle these things on the list. And the reason that I say to do that is that you get to know your own body, your own emotions better because our brains can tell us all kinds of things. In that job where I just went downhill, my brain was telling me, "Work harder, work harder. You can do this. You've done it before." And my body was getting deteriorated and my soul was shrinking, but I wasn't paying attention to that.
I think paying attention to those things and then say, okay, these are the values I was living out. Connection, service, social justice, whatever, compassion. These are the things that I really felt I was living out in that moment. Okay. Now, as I look at my practice, where do I feel those sensations, those physical sensations and those emotions and live out those values? Is it present in my practice? Oh yeah. When I see a mom with a newborn baby and she's in my office and she's in tears and says, "Oh gosh, I feel like a failure as a mom." Now, to me, that hits all my values. So, I sit back and I don't say, "Oh, come on. You were great. You're a great mom. Come on. You do a great job. You'll be fine."
But I sit back and I say, "Wow, tell me about what that feels like. What does it feel like to feel like you're just a failure as a mom?" And then really pay attention and listen. Now that's me. Those are my values. That's the kind of thing. Now, other people may not be like that, but it's important to know what are those things that really make you click? What is your "why" and what are the things associated with that? And then if you can expand the number of experiences in your job where those values are present, and those feelings are present and try to push away those things on the other end of the spectrum which you feel like go against your values and are miserable and you can't stand, then your job satisfaction can increase.
They found with academic physicians, this group one study that was done found that if they can say that 20% of their activities during the course of the week are things that they're passionate about, then they'll deal with the other 80%, no problem. But we don't even have that. We don't have 20% of anything. And then that is what is happening now as more and more physicians are finding that a hundred percent of what they experience is just drudgery.
John: Yeah. I think back when I was burnt out, the way I summed it up was I just started hating my patients because I always said, medicine is fantastic if it wasn't for the patients, which is kind of an oxymoron there, but then you know something is wrong.
Dr. Joe Sherman: Yeah.
John: For sure. I have a pediatrician friend who loves taking care of kids and the families of the kids that have attention deficit disorder. He loves teaching the family. He'll spend an hour if he can do it, it's hard in today's practice. But he's trying to figure out how to do more of that and less of something else. And so far, I think he's been at least a little bit successful. So, that makes sense.
Dr. Joe Sherman: Yeah. Right now, I still do some clinical medicine I fill in for physicians at a clinic where I used to work. And it's a group of physicians that decided to start a nonprofit private practice because they had a mission, a common mission that we all wanted to serve, and we wanted to spend more time with patients. So, we said, okay, we're going to compromise our income a little bit, but we're going to have 45 minutes of child visits. We're going to have 30-minute acute visits and follow ups. We're going to have one hour for every ADHD evaluation.
And then we found that unrecognized autism was a huge issue. And so, we're going to start figuring out how we can be a center of excellence to do autism evaluation. These are things that are possible to do. You have to be a bit creative. You have to really look and say, "How can I look at all possibilities and not just say, oh, I called my friend for residency and it's just as bad for her. So, I'm stuck. I'll just stick it out with the hell?"
John: I spoke with a guest not too long ago, who is seeing a big resurgence of direct contracting, they call DPC and I think it's being driven by the large employers and they're just trying to get rid of the insurance companies and just contract directly with physicians so that they can do the 30-minute, the 45-minute visit. So maybe there's some hope out there. In the meantime, try and focus on what you said in terms of finding those things that most resonate with your vision and your values. So, tell us, you're doing individual coaching too in between the retreats that obviously aren't happening every other weekend or anything.
Dr. Joe Sherman: Yeah. Right.
John: So, give us the whole rundown. What's your website and how does someone contact you if they want to learn more about your coaching or your retreats?
Dr. Joe Sherman: Sure. My website is joeshermanmd.com. Very simple. And if you just plug that in and search it, then you'll find my website. And you can email me directly. It's joe@joeshermanmd.com. And on my website, if you go there, there's an option to schedule a free 30 minutes consultation. And I would say the individual coaching, if somebody is feeling, I mean, there's a variety of things. If you're just feeling like, "Boy, I just want some clarity in trying to make career discernment about what direction to take." That's great. That's a reason for coaching. If you feel like bosh, "I am just burned out completely. I feel like I just don't fit anymore and I don't know what to do. I'm kind of confused." That's a reason for coaching. If I feel like, "Wow, I just transitioned to this new job and I really want to make sure that I get off on the right start and I don't commit to things that I really don't really like doing. And I have that tendency to never say no." That's a good reason for coaching, setting boundaries and so forth. Usually with this consultation, find out a little bit about what the issue is. Talk a little bit about this philosophy of examining your life and then integrating it into your experiences and then coming back and seeing how it worked or didn't work. And decide then whether it makes sense to continue on with individual coaching programs.
John: Sounds good. This episode is probably going to be released sometime in August. And so, I did want to mention that your next retreat is actually going to be held in September. I think the third week of September, something like that. Is that right?
Dr. Joe Sherman: Yes. Correct. It's September 22nd to 25th and it's on Whidbey Island, Washington. It's right off the coast of Seattle. And it's a beautiful, beautiful setting right on the beach with the majestic Olympic mountains in the background, which includes some kayaking and mountain activities.
John: Oh, nice.
Dr. Joe Sherman: Yeah. It's the best time to be in the Pacific Northwest. Everybody hears about the rain in Seattle, but come in September, that's the beautiful time.
John: Excellent. I always think of all those people out in Washington, they seem to be so outdoorsy and fit. I'm in the Midwest where everyone's fat and lazy.
Dr. Joe Sherman: I'm a transplant out here. So, I'm still trying to. My wife is from here, so she's a little bit more focused to the outdoors. I'm doing my best.
John: I would love to be able to just throw a kayak in the lake or the river and hop in and do it. I mean, I've kayaked a couple of times, but when we're living in the Midwest, you got to struggle to get any kind of activity. We live in the cornfield. So, I guess if you want to just jog, you're okay. But you got a lot of options out where you are.
Dr. Joe Sherman: Yeah, there are. Yeah.
John: My listeners, you better try that because it'd be like a vacation. You're going to be gone for two or three days. You actually are going to learn something. You can get CME credit, you're going to have some insights into how to make your life better and then do some sightseeing and get a little exercise all at the same time.
Dr. Joe Sherman: Yeah. And speaking of CME credit, actually, you can get CME credit from individual professional development coaching too. And that's one thing that I tell my clients or potential clients is that they're not category one, but if you look at whatever your state licensing requirements are, you can have a certain number of category two, category three. But for professional development coaching, you can apply CME credit for those for state licensing.
John: Yeah, definitely. It's usually category two and most states will accept that. They don't always require category one for sure. Excellent. Well, this has been fun. I guess we're running out of time. Well, we're over time now, but that's okay. We're having a good time. So, I really appreciate you coming on the show today, Joe. This has been very fun. And I look forward to hearing about what you do over the next few years with this coaching and consulting that you're doing. I appreciate you for being on the podcast today. And with that, I have to say goodbye.
Dr. Joe Sherman: Thanks so much, John. I really appreciate the invitation and chatting with you.
John: It's been my pleasure.
Sign up to receive email reminders, news, and free stuff every week!
Enter your name and email address below and I'll send you reminders each podcast episode, notices about nonclinical jobs, information about free and paid courses, and other curated information just for you.
Transcription PNC Podcast Episode 260
Boost Well-Being by Aligning 'Soul to Role' in Career Selection
John: Today's guest is an accomplished pediatrician. In fact, he's done his pediatric practice all over the world from what I can tell, but really that's not why he's here today, because he's transitioned into being a coach, consultant and retreat facilitator, which we're going to learn about today. So, with that, I would just like to welcome Dr. Joe Sherman. Hello.
Dr. Joe Sherman: Hi John. Thanks so much for having me.
John: It's my pleasure. I'm looking forward to talking and hearing about your burnout, how you transcended that or overcame that and what you're doing now. So, it's going to be a very interesting conversation, I'm sure.
Dr. Joe Sherman: Yeah. Thanks so much. I always enjoy talking about this.
John: Excellent. So now we usually start with a little background. Just give us the short version of your background, your education, clinical work, and definitely touch on some of the things you've done that are a little different from the typical pediatrician.
Dr. Joe Sherman: Sure. I'm an east coaster. I was born and raised in Washington, DC in the city and went away for college at Duke University and then went to Richmond, Virginia at Virginia Commonwealth University, Medical college of Virginia. I did both medical school and residency there in pediatrics and then moved from there back to DC and then began my career as a general pediatrician.
And I would say that the majority of my focus in practice was service to underserved populations of children and families. And my passion really lies in the education and teaching of trainees and bringing the community and the academic center together in trying to link them up. And back then in the late 80s, when I was beginning my practice, most training centers were ivory towers and you never left the building. Now it's a little bit more integrated, but at the time it wasn't.
I worked in many outreach projects where we had teams, interdisciplinary teams to reach out to different populations, pediatric mobile clinics and teams that were based in the community and doing house calls and so forth. In addition to that, I've had stints in Uganda as well as in Bolivia. And I love international health and working with organizations in both of those countries, as well as short term trips to some other Latin American countries.
So, that's about a summary of my clinical experience. And as long as I kept doing that variety of things, I found that I was fulfilled in medicine. But I have to say that pretty much the whole time, even at the beginning of my training, in the back of my mind there was always this thought that came up of "Does this have to be in medicine? Could I be doing some of these things outside of medicine?" Because I always enjoyed athletic coaching and counseling and tutoring and mentoring. And so, those are the things that, especially overseas where you have to kind of wear a lot of hats when resources are very low. That's when I found that I really thrived.
John: Nice. You were sort of going back and forth in some of these activities but apparently from our conversation before we got on the call here, is that you at some point had some episodes where you were pretty burnt out, is that right?
Dr. Joe Sherman: Yes. I would say I was. And I think the classic definition of burnout, this emotional exhaustion dissociation, sense of lack of impact and so forth. At times I had that classical syndrome, I would say. At other times I feel like I was just misplaced, perhaps. It was just the wrong job with the wrong time in my life. And during my time in my practice, I went from being single, to being married without kids to later on being married with kids and little kids and then big kids. Life changes, your situation changes. So therefore, what you're attracted to as far as a practice, a job, an activity is concerned, also changes. I had some minor changes and I always kind of switched jobs I think in those situations and moved on. Opportunities were there.
But then the real crash came when I returned from Bolivia after living there for four years with my family and we raised our little kids there. And returned and tried to plug back into academic medicine here in Seattle. And I just started to go downhill and it was confusing to me. I know that what I had experienced in Bolivia was amazing. I was doing a variety of activities and that fit me well. And yet when I was placed in this clinic in an atmosphere and setting that it seemed like logically, cognitively on paper, would've been the perfect fit. I found myself going downhill. It was confusing to me. I became increasingly anxious. I wanted to work harder to try to fix a broken system. I felt responsible for everybody and everything.
And so, at a time where I was really starting to feel uncertain, it was proposed to me that I was doing such a great job. Why don't I become the medical director of the clinic? And so, like many of us physicians do, when we think something's wrong and we're not feeling too well about our situation, we work harder to try to make it better and try to fix it. And so, I did, and that just made me crash even further.
John: After speaking with so many people about this topic, I think there's an expiration date or something sometimes. Sure, there's medical students, residents they're burned out from day one. They stay burned out and they get fried, but most of us go into it, we're excited. It's interesting. We're at the top of our game because we've just finished our training. I don't know. It's almost like a candle. There's a point where the candle is gone. It's disappeared. The wax evaporated, it burned and there's nothing left And for each of us, medicine is such a fast-changing field that it's really easy to get overwhelmed. And you can only keep that level of intensity for so long. So, I don't know. That's kind of what I'm starting to think about after going back and thinking about my burnout.
Dr. Joe Sherman: Yeah. John, I think as I look back during the time of my training and then my medical practice, medicine has changed dramatically during that time. I mean, not just the evolution of the electronic health record, but also other technology and research and the complexity of medicine has changed. And so, the things that I could keep in my little pocket of that handbook that said, "Oh, I'll just look it up in the Harriet Lane Handbook and tell you what to do." Now it's an enormous amount of information.
John: It is. And I think about this all the time. When I was in med school, literally there were probably 10 medications I had to choose from. A couple of antibiotics, Lasix. Tegnect, the first medicine for ulcers. It didn't exist when I started med school. It's just overwhelming now. There's like a bunch of drugs for COVID. It's just blowing my mind. I can't keep up. Anyway, I'll stop beating that horse.
Dr. Joe Sherman: I'll just say there was just one little vignette very quickly, is that when people talk about HIV. HIV now.
John: Oh yes, exactly.
Dr. Joe Sherman: I had one hour lecture on HIV in my entire medical career, in my entire medical training. And it was by a pathologist who just said there's this strange disease seen in San Francisco. Just want to let you guys know and stay tuned for more. That was it.
John: Wow. Well, I think about that and I look back and I had two patients die of HIV, no treatment whatsoever available for it. And now it's like, okay, we've got these multiple drug pills you take once a day, once a week, whatever. And it's completely controlled. So, it's fantastic. But boy was that frustrating back in the day.
Dr. Joe Sherman: My first pediatric patient, it was a baby who died of perinatal transmission of HIV.
John: That's rough. Okay. Now, you kind of did a reassessment and started to think about whatever the next thing you were going to do when you decided, "Well, maybe I've reached that point." So, tell us about that transition and what you did to prepare for it.
Dr. Joe Sherman: Sure. Like I say, I tried to hang on and make things better. And I was in therapy, seen a psychiatrist just because of anxiety, depression, but still would not let go of this job because it was my identity. And finally, I had to. It was kind of like if I wanted to stay in my marriage, in my family, I just had to do something. So, I did. And it was a time where I stopped and just sat back and said "I need to really reassess where I am in my life and how I got here."
And I came across a book written by Parker Palmer called "Let Your Life Speak." And he wrote about this concept of soul to role that somehow we can examine our lives and see the experiences that we've had and from looking at those experiences we can reflect on that and determine what are those things that really bring us joy in life. What are those things that really bring us to life that make us feel like we are excited?
One of the things that I say is what is some activity that while you're doing it, you wish it would never end because you're having so much fun or you're enjoying it so much? Or what is something that you have done that you say, "I can't wait to get back and do that again?" And then extract the elements of what was present in that time and see how that might fit into a career or your next decision or other things in your life.
Reading that book attracted me to the Center for Courage & Renewal, which is a center that he helped found and group retreats for people who were trying to discern how to live their lives more authentically. And so, I went to a couple of those retreats and found them extremely helpful and decided to train to be a facilitator of those retreats. And that's how I got my start with accompanying health professionals on that journey.
John: Okay. Yeah. Tell us about the retreat concept, maybe the way you're doing it now, or how it's evolved for you. I've always found that group activities can be very helpful because people have the shared experience, but yet they have their own perspective and they've learned and they can learn from one another. So, what's that been like for you? How would you do that? Do you get a group of doctors together?
Dr. Joe Sherman: Yeah. The classic model for the Center for Courage & Renewal is this. Go away to a place for like four days and come together and establish community. It's almost parallel reflection, parallel discernment. And so, everyone is working on their own issues, but you're doing it in a circle of trust, a circle that has a certain guideline you call them touchstones.
Well, the problem is healthcare professionals are very busy. It's really hard for them to get away for that much period of time. So, I tried to adapt it a bit to their situations. I started to do mini retreats for medical teams, inpatient teams, such as palliative care teams or outpatient clinic staff and say, "Hey, let's do a half day retreat or all-day retreat." Or the other thing that I did was, for example, with palliative care teams, can I meet with the team for an hour and a half once a month and have this ongoing reflection on their experiences and how it applies to the direction that they want to take. And this builds team unity and also helps people understand each other on the teams.
Those are types of offerings that I have now, which are those short term, either reflection groups or workshops, as well as the classic getaway and do in that model of going to a place where you can reflect, you can relax, you can rejuvenate, and you can also gain some CME credit for it at the same time. So, we also have those available too.
John: Okay. I think you've got one coming up in a month from what I remember, a month or two. Who would be the ideal member or someone who would come to that? In other words, are you bringing a team from one local spot or are you pulling people from the whole country? And what is the thing that is common to all those people where getting together is going to help them?
Dr. Joe Sherman: Yeah. I have a co-facilitator who's a clinical psychologist who specializes, all of her clients are physicians. These retreats that we have, that we co-facilitate together, we have one in the wintertime in February that's in Florida. And then we have one that's in the early fall on Whidbey Island outside of Seattle, Washington. And these retreats are transformational leadership retreats. And they're worth 25 hours of CME credit, category one credit. And it's really a time for any type of physician, nurse practitioner, PA, medical provider, who wants to examine their practice, their lives in the context of a position that they hold. Perhaps it's a leadership position, either formal or informal within their organizations. And the idea is "I want to examine what brings me life and how I can act more authentically and then how I can transform my organization so that I can provide a space and a culture for everyone to be able to do that."
And one of these big AMA surveys that was done during the pandemic concluded that there were two elements that were associated with resilience of medical providers during the pandemic. And those two elements that had to be present in their organization was one that they felt like there was a shared mission that they felt like they were all in this together. And that that was explicit and lived out.
The second was that they felt valued, that they felt like they were valued by their organization as a member of that organization. And that has implications. The implications are that you're engaged in decision making and the direction that things take. So, those are the topics that we deal with during these retreats as to how to get yourself to examine who you are, why you do what you do, and then how you can bring that to your organization.
John: I find that interesting and I have a question for you about that only because most people that I talk to on my podcast here are people that are ending up leaving medicine. But there's been coaches that I was surprised to find out during the interview that like 80%, 90% of the people they work with actually stay in practice. So, it's how they do the coaching or the people that are coming to them, but that's the whole point is they want to continue in practice.
What I'm hearing from you is that if you can become a leader in one of these organizations, you can continue doing what you're doing now. You may be pulled away and spend more time in leadership and less time seeing one on one patients. But is your feeling that most of these people are there to learn how to stay in practice with a group and support one another and continue doing that for patients?
Dr. Joe Sherman: I would say for these retreats, people come with all kinds of ideas because they're at different stages of their careers. Some people are early on, pretty young. Some people are looking at perhaps retiring and maybe they're burned out. Maybe they need some reason to stay in it, or maybe they're looking at a way to make it work. And making it work may be that they transition a little bit out of clinical medicine and more toward administration or more toward program development or something outside of clinical medicine altogether. It's different for every person I would say.
John: Do you get feedback from the participants later? What's your general sense of their ability to make that change?
Dr. Joe Sherman: Yeah. It's so hard because when I talk to physicians and other clinicians, they feel like they're stuck in a system that is intransient. It just will not change.
John: It's a system.
Dr. Joe Sherman: It's a system problem, right?
John: Yeah.
Dr. Joe Sherman: And usually my response to that is you're right. It is unjust to blame you as an individual physician or other provider. It's unjust to say, "It's all your fault. You just have to shape up, do a little meditation and yoga. You'll be better." That is totally unfair. We are in a broken system. Now, as a result of that, what are you going to do about it? If you are someone who is a political activist and you are a leader, and you're going to really put your energy into changing the system, all the power to you, we need more people like that. If you're not, and you really want to concentrate on taking care of patients or concentrate on teaching or research or whatever it is. Well, then what can you do to fortify yourself to make your own experience more fulfilling? And what can you do with the closest sphere of influence around you? Who do you interact with every day? Because those are the people that can make or break your day.
So, we focus on that. And I would say that when people go through our retreats, as well as my individual coaching, that's what I really focus on is really what is it that drives you and how can you bring that out in other people so that you provide a culture that everyone feels supported? They feel like they're valued, and they feel like they're in the same mission.
John: And when I left medicine, I went into administration at a hospital, became a chief medical officer. And so, I was kind of on a dark side in a way. But I think that while I was doing it, I was actually helping the physicians. Even at the base level of saying, "You know what? You're not getting paid enough. We're going to give you a raise" The CFO was not going to volunteer to do that. The CEO wasn't either. And so, I'm always encouraging people to get involved in leadership. If you're frustrated, you can go one of two ways. You can bail on the whole thing, or you can get involved and change it somewhat.
Dr. Joe Sherman: Yeah. I think what they used to say is that the MDs that go to administration went to the dark side and now we don't like them anymore because they're the bad guys. But it's almost like administrators and clinicians live in these two different cultures. And never the twain shall meet or get along, but I've been in situations, especially with smaller organizations where that shared mission is explicit and discussed amongst administrators as well as clinicians. And when you do that, then you want to learn from the other person.
And tell me about your experience. Tell me about the pressures as an administrator that you have to keep the bottom line going. And I'll listen to you as long as you listen to me about the hassles I have to do with trying to check all the boxes you want me to check. And I think if people are able to see each other as humans and move forward in that, then I think they can get along. And I also believe that money is not always the answer and it's turning out I think especially during this pandemic, that time and the quality of how you spend your time is so much more valuable to people.
John: Right. Absolutely. Anecdotally, I think there's evidence that large systems that are actually run by physicians, that understand one another, have more engagement with the other physicians and actually their burnout levels are lower. So, that's why I encourage physicians to get into those leadership positions because yeah, you can improve it even within a broken system.
Dr. Joe Sherman: Yeah. And I think sometimes it's intimidating and it's interesting because when I do individual coaching, individual coaching in the corporate business world is thought to be a perk. It's thought to be, "Wow, I got a coach. This is great."
John: That's right.
Dr. Joe Sherman: But for physicians, it's thought to be a little bit kind of like remedial, like you're behind in your charts, you're causing a problem in the OR, we need to coach you up so that you act better. So, when coaches, even when they get to leadership positions, sometimes they think "Coach? Oh, gosh. I don't want you to, because I just need to learn how to be an administrator. I need to learn business." And it may be true. You need to learn the vocabulary, but you're not in the room. There's plenty of business people in that room. They need people who can tell them this is the implication and the impact of that decision on the clinicians when you make that change.
John: Yeah. So many of them just really have no idea if they've never been a clinician at any level. There's a lot of nurses that run hospitals and that kind of thing. But when you have just the MBA, it's doing it. They really don't understand the physician-patient relationship or what a nurse really truly does. Okay. So now I want to pick your brain a little bit more because you mentioned the book earlier and you mentioned Let Your Life Speak and you mentioned Soul to Role.
Dr. Joe Sherman: Yeah, that's correct.
John: Which you explained, but can you give us a little bit more about how I might be able to figure that out? I'm one of those people like, I don't know how I feel and how am I going to figure out what I really enjoy doing?
Dr. Joe Sherman: Yeah. As physicians, we're very much in our heads all the time. And the strangest thing is that we deal with the body. I mean, that's what we're dealing with. We dissected it. We do study physiology, all that stuff. We're not very in touch with our own bodies. And we're not very much in touch with our emotions, our soul, whatever you want to call it.
A lot of times, I think "What are you talking about this solar role? What is it?" Well, one thing is to say, and what we talked about before is think of an experience that you've had where you've felt those things that I said, "I wish it would never end or I can't wait to do it again." And then you look at it and you say, "Wow, who was involved? What was the setting? What was it? What are the values I was living out? What were the feelings? How did it feel in my body? What were the emotions I felt?"
Now I have to say, for me, you have to be pretty elementary with physicians. They say with myself too. So, I have a list of emotions, a list of feelings, a list of body sensations. Pick something, circle these things on the list. And the reason that I say to do that is that you get to know your own body, your own emotions better because our brains can tell us all kinds of things. In that job where I just went downhill, my brain was telling me, "Work harder, work harder. You can do this. You've done it before." And my body was getting deteriorated and my soul was shrinking, but I wasn't paying attention to that.
I think paying attention to those things and then say, okay, these are the values I was living out. Connection, service, social justice, whatever, compassion. These are the things that I really felt I was living out in that moment. Okay. Now, as I look at my practice, where do I feel those sensations, those physical sensations and those emotions and live out those values? Is it present in my practice? Oh yeah. When I see a mom with a newborn baby and she's in my office and she's in tears and says, "Oh gosh, I feel like a failure as a mom." Now, to me, that hits all my values. So, I sit back and I don't say, "Oh, come on. You were great. You're a great mom. Come on. You do a great job. You'll be fine."
But I sit back and I say, "Wow, tell me about what that feels like. What does it feel like to feel like you're just a failure as a mom?" And then really pay attention and listen. Now that's me. Those are my values. That's the kind of thing. Now, other people may not be like that, but it's important to know what are those things that really make you click? What is your "why" and what are the things associated with that? And then if you can expand the number of experiences in your job where those values are present, and those feelings are present and try to push away those things on the other end of the spectrum which you feel like go against your values and are miserable and you can't stand, then your job satisfaction can increase.
They found with academic physicians, this group one study that was done found that if they can say that 20% of their activities during the course of the week are things that they're passionate about, then they'll deal with the other 80%, no problem. But we don't even have that. We don't have 20% of anything. And then that is what is happening now as more and more physicians are finding that a hundred percent of what they experience is just drudgery.
John: Yeah. I think back when I was burnt out, the way I summed it up was I just started hating my patients because I always said, medicine is fantastic if it wasn't for the patients, which is kind of an oxymoron there, but then you know something is wrong.
Dr. Joe Sherman: Yeah.
John: For sure. I have a pediatrician friend who loves taking care of kids and the families of the kids that have attention deficit disorder. He loves teaching the family. He'll spend an hour if he can do it, it's hard in today's practice. But he's trying to figure out how to do more of that and less of something else. And so far, I think he's been at least a little bit successful. So, that makes sense.
Dr. Joe Sherman: Yeah. Right now, I still do some clinical medicine I fill in for physicians at a clinic where I used to work. And it's a group of physicians that decided to start a nonprofit private practice because they had a mission, a common mission that we all wanted to serve, and we wanted to spend more time with patients. So, we said, okay, we're going to compromise our income a little bit, but we're going to have 45 minutes of child visits. We're going to have 30-minute acute visits and follow ups. We're going to have one hour for every ADHD evaluation.
And then we found that unrecognized autism was a huge issue. And so, we're going to start figuring out how we can be a center of excellence to do autism evaluation. These are things that are possible to do. You have to be a bit creative. You have to really look and say, "How can I look at all possibilities and not just say, oh, I called my friend for residency and it's just as bad for her. So, I'm stuck. I'll just stick it out with the hell?"
John: I spoke with a guest not too long ago, who is seeing a big resurgence of direct contracting, they call DPC and I think it's being driven by the large employers and they're just trying to get rid of the insurance companies and just contract directly with physicians so that they can do the 30-minute, the 45-minute visit. So maybe there's some hope out there. In the meantime, try and focus on what you said in terms of finding those things that most resonate with your vision and your values. So, tell us, you're doing individual coaching too in between the retreats that obviously aren't happening every other weekend or anything.
Dr. Joe Sherman: Yeah. Right.
John: So, give us the whole rundown. What's your website and how does someone contact you if they want to learn more about your coaching or your retreats?
Dr. Joe Sherman: Sure. My website is joeshermanmd.com. Very simple. And if you just plug that in and search it, then you'll find my website. And you can email me directly. It's joe@joeshermanmd.com. And on my website, if you go there, there's an option to schedule a free 30 minutes consultation. And I would say the individual coaching, if somebody is feeling, I mean, there's a variety of things. If you're just feeling like, "Boy, I just want some clarity in trying to make career discernment about what direction to take." That's great. That's a reason for coaching. If you feel like bosh, "I am just burned out completely. I feel like I just don't fit anymore and I don't know what to do. I'm kind of confused." That's a reason for coaching. If I feel like, "Wow, I just transitioned to this new job and I really want to make sure that I get off on the right start and I don't commit to things that I really don't really like doing. And I have that tendency to never say no." That's a good reason for coaching, setting boundaries and so forth. Usually with this consultation, find out a little bit about what the issue is. Talk a little bit about this philosophy of examining your life and then integrating it into your experiences and then coming back and seeing how it worked or didn't work. And decide then whether it makes sense to continue on with individual coaching programs.
John: Sounds good. This episode is probably going to be released sometime in August. And so, I did want to mention that your next retreat is actually going to be held in September. I think the third week of September, something like that. Is that right?
Dr. Joe Sherman: Yes. Correct. It's September 22nd to 25th and it's on Whidbey Island, Washington. It's right off the coast of Seattle. And it's a beautiful, beautiful setting right on the beach with the majestic Olympic mountains in the background, which includes some kayaking and mountain activities.
John: Oh, nice.
Dr. Joe Sherman: Yeah. It's the best time to be in the Pacific Northwest. Everybody hears about the rain in Seattle, but come in September, that's the beautiful time.
John: Excellent. I always think of all those people out in Washington, they seem to be so outdoorsy and fit. I'm in the Midwest where everyone's fat and lazy.
Dr. Joe Sherman: I'm a transplant out here. So, I'm still trying to. My wife is from here, so she's a little bit more focused to the outdoors. I'm doing my best.
John: I would love to be able to just throw a kayak in the lake or the river and hop in and do it. I mean, I've kayaked a couple of times, but when we're living in the Midwest, you got to struggle to get any kind of activity. We live in the cornfield. So, I guess if you want to just jog, you're okay. But you got a lot of options out where you are.
Dr. Joe Sherman: Yeah, there are. Yeah.
John: My listeners, you better try that because it'd be like a vacation. You're going to be gone for two or three days. You actually are going to learn something. You can get CME credit, you're going to have some insights into how to make your life better and then do some sightseeing and get a little exercise all at the same time.
Dr. Joe Sherman: Yeah. And speaking of CME credit, actually, you can get CME credit from individual professional development coaching too. And that's one thing that I tell my clients or potential clients is that they're not category one, but if you look at whatever your state licensing requirements are, you can have a certain number of category two, category three. But for professional development coaching, you can apply CME credit for those for state licensing.
John: Yeah, definitely. It's usually category two and most states will accept that. They don't always require category one for sure. Excellent. Well, this has been fun. I guess we're running out of time. Well, we're over time now, but that's okay. We're having a good time. So, I really appreciate you coming on the show today, Joe. This has been very fun. And I look forward to hearing about what you do over the next few years with this coaching and consulting that you're doing. I appreciate you for being on the podcast today. And with that, I have to say goodbye.
Dr. Joe Sherman: Thanks so much, John. I really appreciate the invitation and chatting with you.
John: It's been my pleasure.
Sign up to receive email reminders, news, and free stuff every week!
Enter your name and email address below and I'll send you reminders each podcast episode, notices about nonclinical jobs, information about free and paid courses, and other curated information just for you.
Disclaimers:
Many of the links that I refer you to are affiliate links. That means that I receive a payment from the seller if you purchase the affiliate item using my link. Doing so has no effect on the price you are charged. And I only promote products and services that I believe are of high quality and will be useful to you.
The opinions expressed here are mine and my guest’s. While the information provided on the podcast is true and accurate to the best of my knowledge, there is no express or implied guarantee that using the methods discussed here will lead to success in your career, life, or business.
The information presented on this blog and related podcast is for entertainment and/or informational purposes only. I do not provide medical, legal, tax, or emotional advice. If you take action on the information provided on the blog or podcast, it is at your own risk. Always consult an attorney, accountant, career counselor, or other professional before making any major decisions about your career.

Leave A Comment
You must be logged in to post a comment.